Hot Flashes, Heart Health, and Hormones: Rethinking Menopause Care
Menopause, a natural transition marking the end of a woman’s reproductive years, is often associated with uncomfortable symptoms like hot flashes. However, the impact of this hormonal shift extends far beyond fleeting moments of intense heat. Emerging research reveals a crucial link between menopause, heart health, and hormonal changes, demanding a re-evaluation of how we approach menopause care. This article explores this vital connection, offering insights into managing symptoms and safeguarding cardiovascular well-being during this significant life stage.
Understanding the Hormonal Shift and its Cardiovascular Implications
Menopause is characterized by a decline in estrogen, a hormone crucial for cardiovascular health. Estrogen plays several protective roles:
- Blood vessel function: Estrogen helps maintain healthy blood vessel elasticity and prevents the build-up of plaque.
- Cholesterol levels: It contributes to favorable cholesterol profiles, reducing the risk of heart disease.
- Blood clotting: Estrogen influences blood clotting mechanisms, decreasing the risk of thrombosis.
The decrease in estrogen during menopause can reverse these protective effects, increasing a woman’s risk of:
- High blood pressure
- High cholesterol
- Heart disease
- Stroke
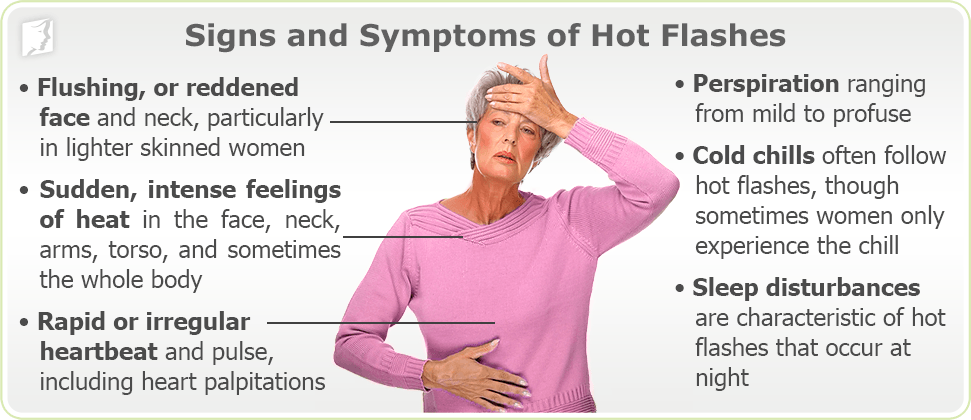
The Hot Flash Connection: More Than Just Discomfort
While seemingly unrelated, hot flashes are also linked to cardiovascular health. The vasomotor symptoms (sudden dilation and constriction of blood vessels) that cause hot flashes might also contribute to long-term vascular damage. Further research is needed to fully understand this connection, but it highlights the importance of comprehensive menopause management.
Rethinking Menopause Care: A Holistic Approach
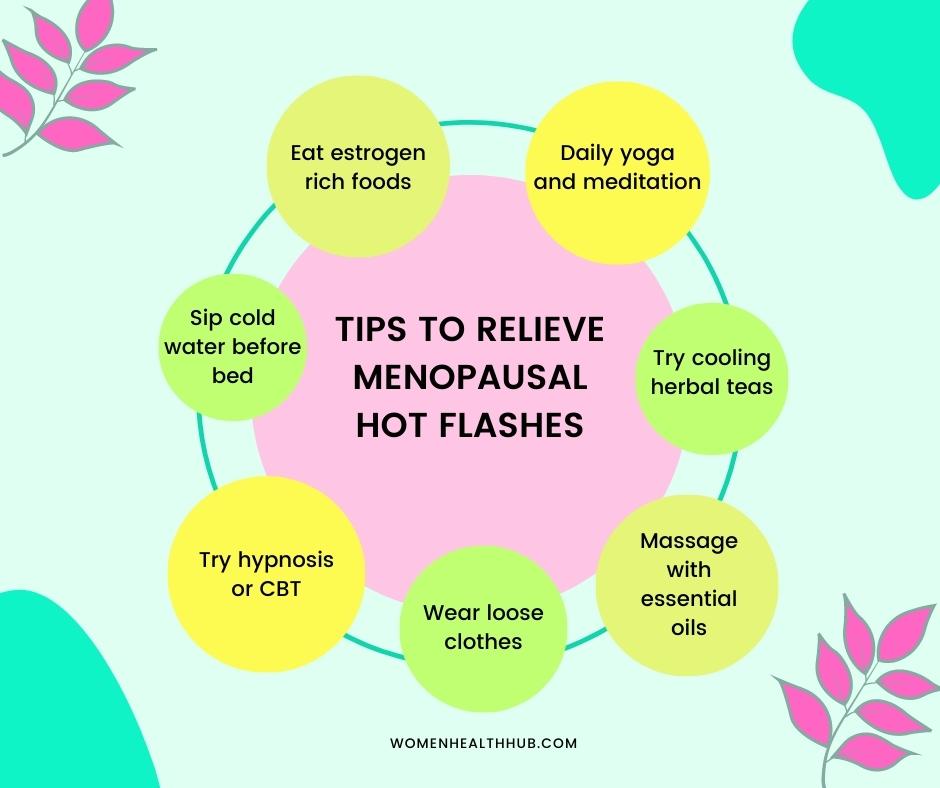
Traditional menopause care often focuses solely on managing symptoms like hot flashes. However, a holistic approach that prioritizes cardiovascular health is essential. This includes:
Lifestyle modifications: Adopting a heart-healthy lifestyle is paramount. This involves:
- Regular exercise: Aim for at least 150 minutes of moderate-intensity aerobic activity per week.
- Balanced diet: Focus on fruits, vegetables, whole grains, and lean protein. Limit saturated and trans fats, sodium, and added sugars.
- Weight management: Maintaining a healthy weight reduces cardiovascular risk.
- Stress reduction: Practice stress-management techniques like yoga, meditation, or deep breathing.
- Smoking cessation: Quitting smoking significantly reduces heart disease risk.
Hormone therapy (HT): HT can alleviate menopausal symptoms and offer some cardiovascular protection, but it’s crucial to discuss the risks and benefits with a healthcare provider. HT is not suitable for everyone.
Alternative therapies: Some women find relief from menopausal symptoms through alternative therapies like acupuncture, herbal remedies, or cognitive behavioral therapy (CBT). Always consult your doctor before trying new therapies.
Regular check-ups: Regular visits to your doctor for blood pressure, cholesterol, and other cardiovascular risk factor monitoring are crucial.
Beyond the Symptoms: Long-Term Cardiovascular Health
The impact of menopause on heart health extends beyond the immediate menopausal years. Women need to be proactive in managing their cardiovascular health throughout their lives, paying particular attention to risk factors during and after menopause. Early detection and intervention are key to preventing future cardiovascular events.
Conclusion: A Proactive Approach to a Healthy Future
Menopause is a significant life transition, and understanding its impact on both immediate symptoms and long-term health is crucial. By adopting a holistic approach that addresses both hot flashes and cardiovascular health, women can navigate this phase with greater comfort and significantly reduce their risk of future heart problems. Open communication with your healthcare provider is essential to develop a personalized management plan that best suits your individual needs and risk factors.
Frequently Asked Questions (FAQs)
Q1: Are all women at increased risk of heart disease during menopause?
A1: While menopause increases the risk for many women, individual risk varies based on factors like family history, pre-existing conditions, and lifestyle choices.
Q2: Is hormone therapy always the best option for managing menopausal symptoms?
A2: No. HT has potential benefits and risks, and its suitability depends on individual circumstances. A doctor should assess the risks and benefits before recommending HT.
Q3: Can diet and exercise truly impact heart health during menopause?
A3: Absolutely. Lifestyle modifications are crucial for mitigating the cardiovascular risks associated with menopause. A healthy diet and regular exercise are cornerstones of heart health at any age.
Q4: What are the warning signs of a heart attack in women?
A4: Women may experience different symptoms than men, including shortness of breath, unusual fatigue, back or jaw pain, and nausea. If you experience any unusual symptoms, seek immediate medical attention.
Q5: When should I start talking to my doctor about menopause?
A5: It’s beneficial to start discussing menopause with your doctor well in advance of the expected onset of symptoms, ideally in your 40s, to proactively manage potential health risks.