Lung Cancer Corrupts Immune Cells at Their Source: A New Understanding of Immunosuppression
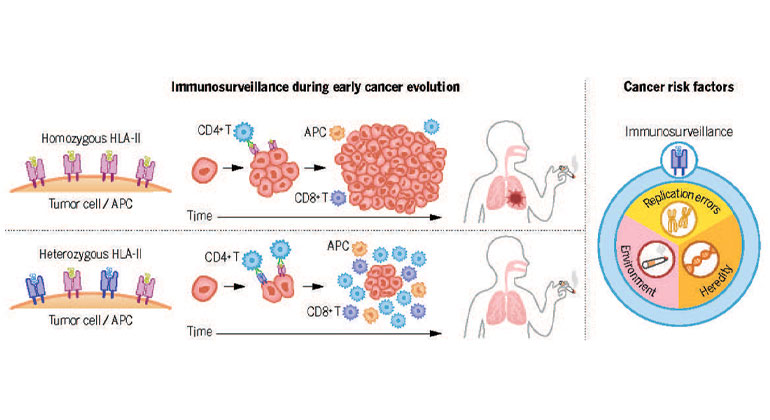
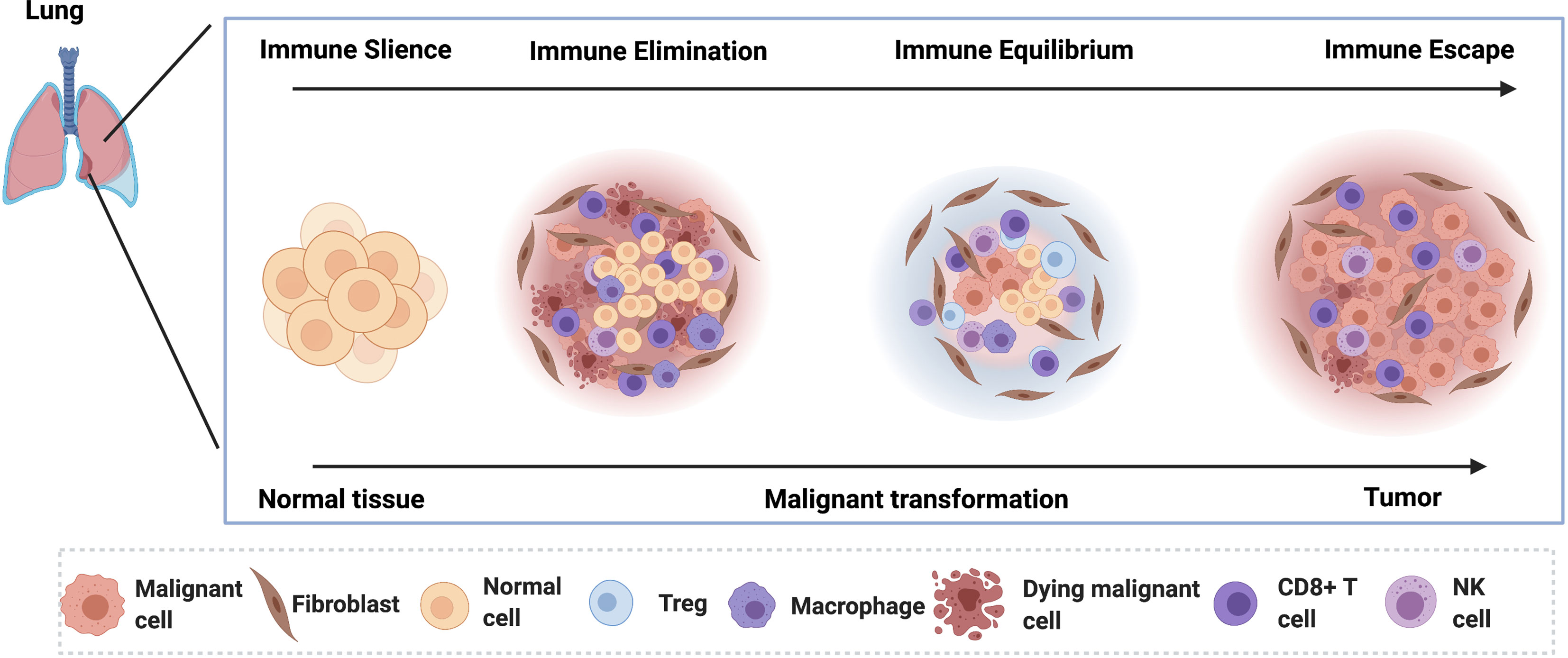
Lung cancer, a leading cause of cancer-related deaths worldwide, is notorious for its ability to evade the body’s immune system. While immunotherapy has revolutionized cancer treatment, its effectiveness in lung cancer is often limited. Recent research sheds light on a crucial mechanism: lung cancer doesn’t just suppress the immune response; it actively corrupts immune cells at their very source – the bone marrow. This discovery offers a potential new avenue for developing more effective therapies.
The Bone Marrow: A Compromised Fortress
The bone marrow is the body’s primary factory for immune cells, including crucial players like T cells and B cells. These cells are essential for recognizing and destroying cancer cells. However, lung cancer can disrupt this vital process in several ways:
- Altered Hematopoiesis: Lung cancer can interfere with the normal production and maturation of immune cells within the bone marrow. This leads to a reduced number of functional immune cells circulating in the bloodstream, weakening the body’s overall defense.
- Immune Cell Dysfunction: Even if immune cells are produced, lung cancer can alter their functionality. This means that even the cells that do make it into circulation might be less effective at targeting and destroying cancer cells. They may become exhausted, anergic (unable to respond), or even promote tumor growth.
- Myeloid-Derived Suppressor Cells (MDSCs): Lung cancer often leads to an increase in MDSCs, a type of immune cell that actively suppresses the anti-tumor activity of other immune cells. These cells act as brakes on the immune system, allowing the cancer to proliferate unchecked.
The Role of Cancer-Associated Fibroblasts (CAFs)
Research points to the significant role of Cancer-Associated Fibroblasts (CAFs) in mediating this bone marrow disruption. CAFs are a type of stromal cell found within the tumor microenvironment. They communicate with the bone marrow through various signaling molecules, essentially sending messages that disrupt normal immune cell development and function. This communication pathway represents a critical target for therapeutic intervention.
Implications for Treatment and Future Research
Understanding how lung cancer corrupts immune cells at their source opens exciting possibilities for improving cancer treatment. This knowledge suggests that targeting the bone marrow and the communication pathways between the tumor and the bone marrow could be crucial for enhancing the effectiveness of existing immunotherapies and developing novel therapeutic strategies. Future research will likely focus on:
- Identifying specific signaling molecules involved in the communication between the tumor and the bone marrow.
- Developing targeted therapies to block these signaling pathways and restore normal immune cell production and function.
- Combining bone marrow-targeted therapies with existing immunotherapies for a synergistic effect.
Conclusion
The discovery that lung cancer actively corrupts immune cells at their source in the bone marrow significantly advances our understanding of cancer immunosuppression. This knowledge paves the way for innovative therapeutic approaches that target the root cause of immune dysfunction, potentially leading to more effective treatments and improved outcomes for lung cancer patients. Future research focusing on the specific mechanisms involved and the development of targeted therapies holds immense promise for revolutionizing lung cancer treatment.
FAQs
Q: Can bone marrow transplants help treat lung cancer-induced immune suppression? A: While bone marrow transplants are used for certain types of cancers and blood disorders, their role in treating lung cancer-induced immune suppression is still under investigation. Further research is needed to determine their effectiveness and feasibility.
Q: Are there currently any treatments targeting this bone marrow disruption? A: Not yet, but research is actively exploring this area. Many clinical trials are investigating novel therapies aimed at restoring normal immune cell function.
Q: How does this discovery impact the use of immunotherapy in lung cancer? A: This discovery highlights the importance of understanding the tumor microenvironment and its influence on the immune system. It suggests that combining immunotherapy with therapies targeting bone marrow dysfunction might significantly improve the effectiveness of immunotherapy in lung cancer.
Q: Is this research applicable to other types of cancer? A: While this research focuses on lung cancer, the principle of cancer-induced bone marrow disruption may apply to other cancers as well. Further research is needed to determine the extent of this phenomenon across different cancer types.
Q: Where can I find more information on clinical trials related to this research? A: You can find information on clinical trials related to lung cancer and immunotherapy through resources like ClinicalTrials.gov and the websites of major cancer research institutions.