Lung Cancer Rewires Bone Marrow Immune Cells to Weaken Body Defenses
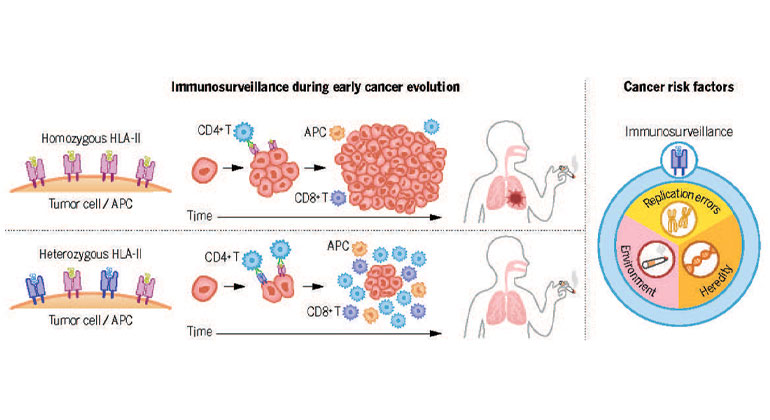
Lung cancer, a leading cause of cancer-related deaths globally, is notorious for its aggressive nature and ability to evade the body’s immune system. Recent research sheds light on a cunning strategy employed by this deadly disease: reprogramming bone marrow immune cells to suppress the very defenses designed to combat it. This article delves into the complex interplay between lung cancer, bone marrow, and the immune system, exploring how this rewiring contributes to cancer progression and potential therapeutic implications.
The Bone Marrow: A Crucial Player in Immunity
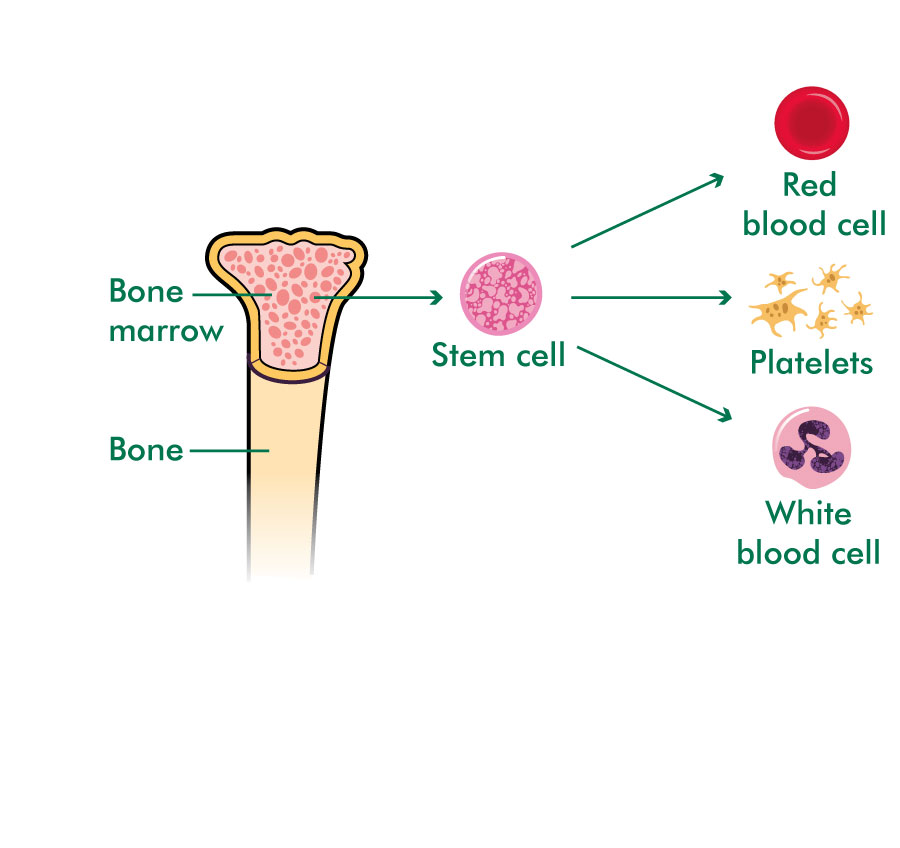
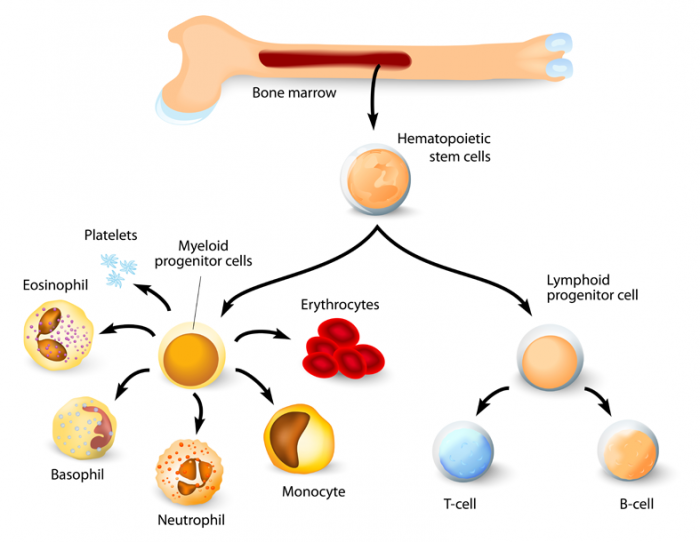
The bone marrow serves as the primary site of hematopoiesis, the production of blood cells, including crucial components of the immune system such as lymphocytes (T cells and B cells) and myeloid cells (neutrophils, macrophages, etc.). These cells are vital for recognizing and eliminating cancerous cells. A healthy immune system relies on the efficient generation and deployment of these cells.
How Lung Cancer Subverts the Bone Marrow
Lung cancer doesn’t simply coexist passively with the bone marrow; it actively manipulates it. Research indicates that lung cancer cells release various factors that alter the bone marrow microenvironment. This disruption leads to:
- Dysregulated hematopoiesis: The production of immune cells becomes imbalanced, favoring the generation of immunosuppressive cells over those with anti-cancer activity. This shift weakens the body’s ability to fight the cancer.
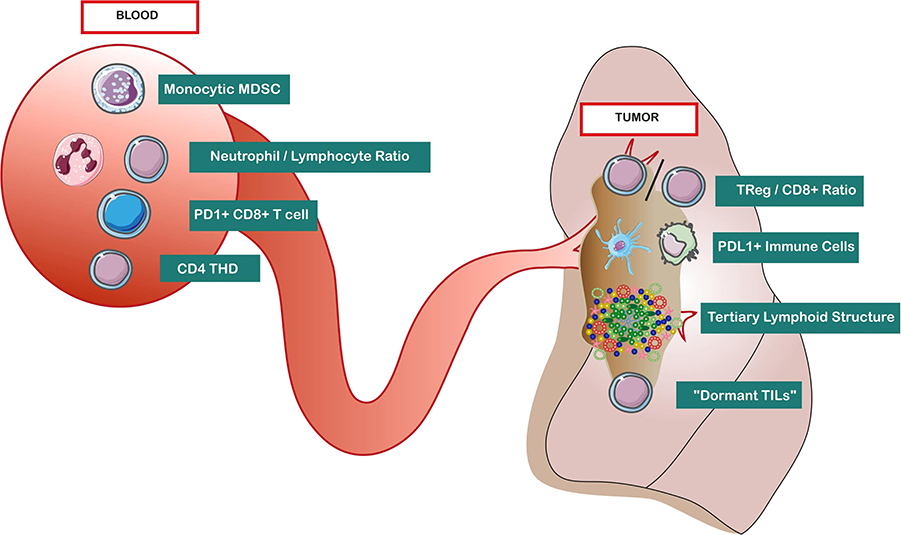
- Impaired immune cell function: Even the immune cells that are produced may be functionally compromised, exhibiting reduced ability to recognize and attack cancer cells.
- Increased production of myeloid-derived suppressor cells (MDSCs): These cells actively suppress the activity of T cells, a key component of the anti-tumor immune response. Lung cancer leverages this to create a more tolerant environment for its growth.
- Altered cytokine production: The balance of cytokines (signaling molecules) within the bone marrow is disrupted, further promoting immunosuppression and hindering the immune response.
Implications for Cancer Progression and Treatment
The bone marrow’s manipulation by lung cancer significantly impacts disease progression and treatment outcomes. A weakened immune system allows the cancer to grow unchecked, leading to metastasis (spread to other parts of the body) and a poorer prognosis. This also explains why some patients respond poorly to immunotherapy, a treatment designed to boost the body’s immune response against cancer.
Targeting the Bone Marrow: Future Therapeutic Strategies
Understanding the mechanisms by which lung cancer hijacks the bone marrow opens avenues for novel therapeutic strategies. Researchers are exploring ways to:
- Restore balanced hematopoiesis: This could involve targeting the factors released by lung cancer cells that disrupt bone marrow function.
- Enhance immune cell function: Strategies to improve the activity of anti-tumor immune cells, even in the face of immunosuppressive factors, are being investigated.
- Deplete MDSCs: Reducing the number of MDSCs in the bone marrow could restore the balance of immune cells and enhance anti-cancer immunity.
Conclusion
The discovery that lung cancer rewires bone marrow immune cells provides crucial insights into the disease’s aggressive nature and its ability to evade immune surveillance. By unraveling the complex interactions between lung cancer and the bone marrow, researchers are paving the way for the development of more effective therapies that target this critical aspect of cancer progression. Further research is crucial to translate these findings into tangible improvements in patient care and survival rates.
FAQs
Q: Can lung cancer spread to the bone marrow? A: Yes, lung cancer can metastasize to the bone marrow, but the effects described here are primarily about the cancer manipulating the bone marrow from a distance, influencing the type and function of immune cells produced.
Q: How is this different from bone marrow suppression caused by chemotherapy? A: Chemotherapy can suppress bone marrow function as a side effect, impacting the production of all blood cells, including immune cells. The mechanism described here is different; lung cancer actively rewires the bone marrow to favor immunosuppression.
Q: Are there current treatments targeting this bone marrow manipulation? A: While no treatments specifically target this rewiring, research is ongoing, and some immunotherapies indirectly address this by boosting overall immune function.
Q: Is this phenomenon unique to lung cancer? A: No, other cancers are also known to manipulate the bone marrow microenvironment to suppress the immune system, although the specific mechanisms may vary.
Q: What can I do to support my bone marrow health? A: Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking, can generally support overall health, including bone marrow function. However, this is not a preventative measure against lung cancer or its effects on the bone marrow.