Lung Cancer Tumor Microenvironment Reveals Immune Escape and New Therapy Targets
Lung cancer remains a leading cause of cancer-related deaths worldwide. While significant advancements have been made in treatment, the disease’s complexity, particularly its ability to evade the immune system, continues to pose a significant challenge. Recent research focusing on the lung cancer tumor microenvironment (TME) is shedding light on these evasion mechanisms and revealing promising new therapeutic targets. This article explores the crucial role of the TME in lung cancer progression and the potential for novel therapies based on these findings.
Understanding the Lung Cancer Tumor Microenvironment
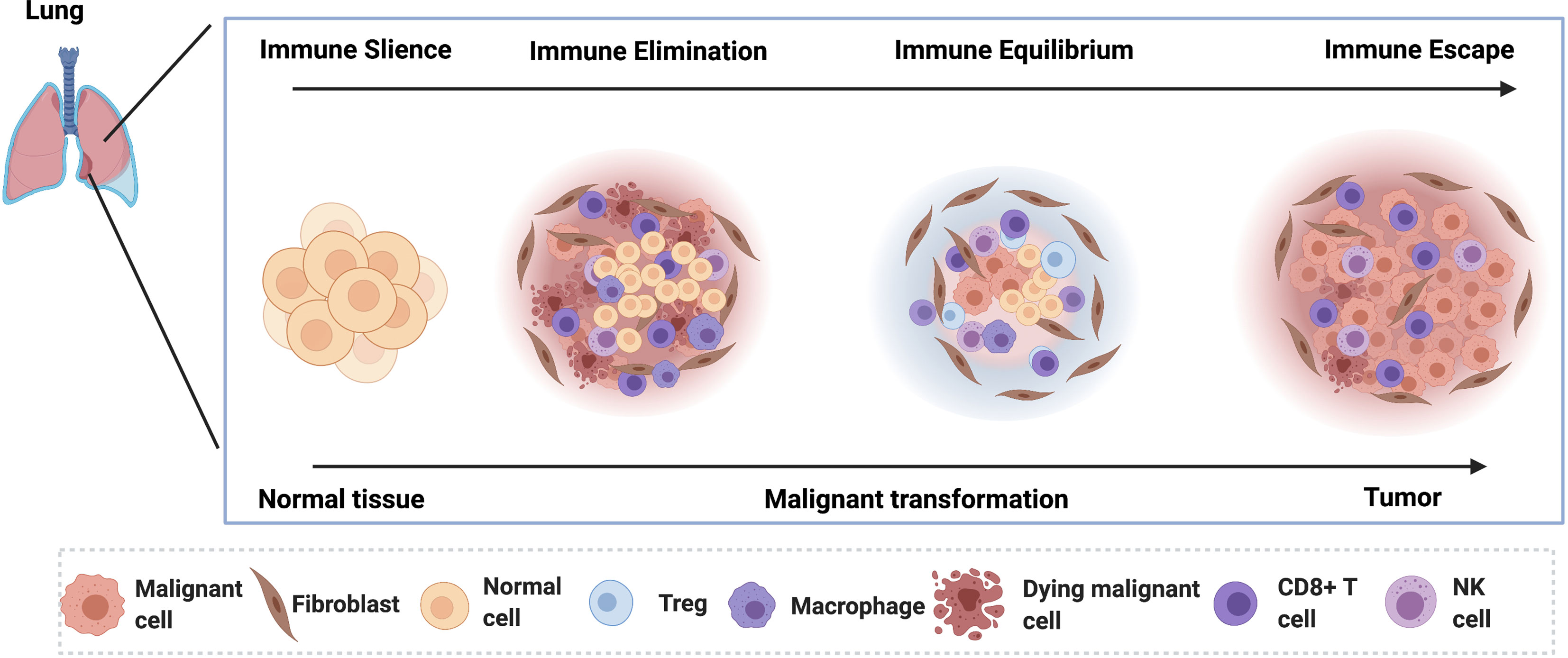
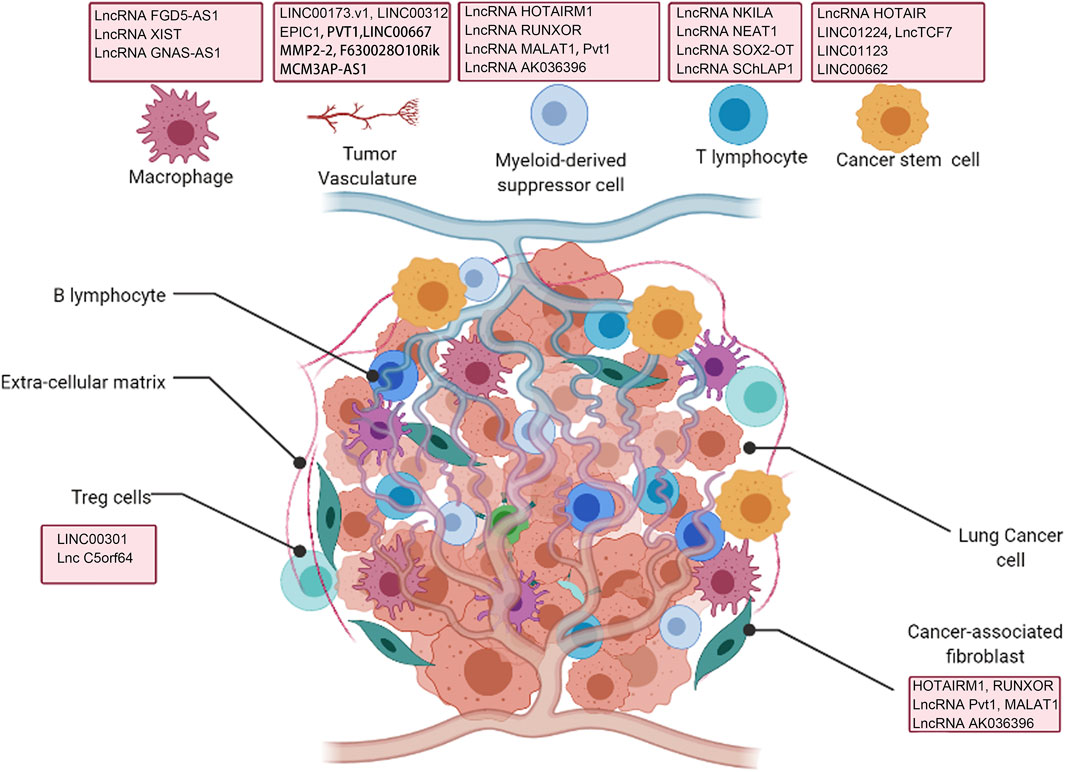
The TME is the complex ecosystem surrounding a tumor, comprising cancer cells, immune cells, fibroblasts, blood vessels, and the extracellular matrix (ECM). This intricate network plays a pivotal role in tumor growth, metastasis, and response to therapy. In lung cancer, the TME is often characterized by:
- Immune suppression: The TME can actively suppress the anti-tumor immune response, allowing cancer cells to proliferate unchecked. This involves the recruitment of immunosuppressive cells like myeloid-derived suppressor cells (MDSCs) and regulatory T cells (Tregs).
- Angiogenesis: The formation of new blood vessels (angiogenesis) within the TME provides tumors with the nutrients and oxygen necessary for growth and metastasis.
- Extracellular matrix remodeling: The ECM, a supportive scaffold for cells, undergoes significant remodeling in the TME, contributing to tumor invasion and metastasis.
- Metabolic alterations: Cancer cells within the TME often exhibit altered metabolic pathways, allowing them to thrive even in nutrient-poor conditions.
Immune Escape Mechanisms in the Lung Cancer TME
A key characteristic of the lung cancer TME is its ability to facilitate immune escape. Cancer cells employ various strategies to evade detection and destruction by the immune system:
- PD-L1 expression: Programmed death-ligand 1 (PD-L1) is a protein expressed by some cancer cells that binds to PD-1 receptors on T cells, inhibiting their ability to kill cancer cells. This is a major mechanism of immune evasion targeted by immune checkpoint inhibitors.
- Recruitment of immunosuppressive cells: As mentioned earlier, the TME attracts MDSCs and Tregs, which actively suppress the anti-tumor immune response.
- Altered antigen presentation: Cancer cells can alter the presentation of their antigens, making them less recognizable to the immune system.
Novel Therapy Targets Emerging from TME Research
Understanding the intricacies of the lung cancer TME has opened up new avenues for therapeutic intervention. Research is focusing on:
- Immune checkpoint inhibitors beyond PD-1/PD-L1: Targeting other immune checkpoints, such as CTLA-4 and LAG-3, is showing promise in overcoming immune suppression.
- Targeting immunosuppressive cells: Strategies aimed at depleting or inhibiting MDSCs and Tregs are under investigation.
- Anti-angiogenic therapies: Blocking the formation of new blood vessels can starve tumors of essential nutrients and hinder their growth and metastasis.
- Targeting ECM remodeling: Modulating the ECM can improve the infiltration of immune cells and enhance the efficacy of other therapies.
- Metabolic therapies: Targeting the altered metabolic pathways of cancer cells can selectively impair their growth and survival.
Conclusion
The lung cancer TME is a complex and dynamic ecosystem that plays a critical role in tumor progression and immune evasion. By unraveling the intricate interactions within the TME, researchers are identifying novel therapeutic targets and strategies to improve the treatment of lung cancer. Further research is crucial to translate these findings into effective clinical therapies and improve patient outcomes. The focus on personalized medicine, tailoring treatments to the specific characteristics of a patient’s TME, holds significant promise for the future of lung cancer treatment.
Frequently Asked Questions (FAQs)
Q1: What is the tumor microenvironment (TME)? A1: The TME is the complex network of cells, molecules, and structures surrounding a tumor, influencing its growth, metastasis, and response to treatment.
Q2: How does the TME contribute to immune escape in lung cancer? A2: The TME promotes immune escape through mechanisms such as PD-L1 expression, recruitment of immunosuppressive cells, and altered antigen presentation.
Q3: What are some novel therapies targeting the lung cancer TME? A3: Novel therapies include immune checkpoint inhibitors beyond PD-1/PD-L1, targeting immunosuppressive cells, anti-angiogenic therapies, and metabolic therapies.
Q4: Is research on the TME leading to personalized medicine approaches? A4: Yes, understanding the unique characteristics of a patient’s TME allows for the development of personalized therapies tailored to their specific tumor.
Q5: What are the future directions of research in lung cancer TME? A5: Future research will focus on further characterizing the TME’s complexity, identifying additional therapeutic targets, and developing combination therapies that effectively target multiple components of the TME.