One Cancer Patient’s Struggle to Get Vaccinated Highlights Challenges Across Healthcare Providers
The journey through cancer treatment is arduous, filled with complex medical decisions and often, a heightened vulnerability to infections. For cancer patients, vaccinations are crucial, offering vital protection against preventable diseases like influenza and pneumonia. However, obtaining these life-saving vaccinations isn’t always straightforward. The experience of one individual navigating this process reveals a complex web of challenges that can impact access to care, highlighting issues across various healthcare providers – from doctors and nurses to pharmacies and clinics.
This article delves into the difficulties faced by cancer patients seeking vaccinations, exploring the systemic hurdles that can impede their access to essential preventative care. We’ll examine the roles of different healthcare providers and the specific areas where inefficiencies and communication breakdowns can occur, ultimately impacting patient well-being.
The Patient’s Perspective: A Difficult Road to Immunity
Imagine facing a cancer diagnosis, undergoing grueling treatments, and then struggling to access a simple vaccination. This reality is far too common. The challenges often begin with a lack of clear guidance and coordination.
- Communication Breakdown: Patients may receive conflicting information from different healthcare providers, leading to confusion about which vaccines are recommended, when they should be administered, and where they can be obtained.
- Specialized Needs: Cancer patients often have unique needs. Their immune systems are frequently compromised, requiring careful consideration of vaccine types, dosages, and timing. This can make vaccination planning more complex than for the general population.
- Navigating Multiple Providers: Cancer care typically involves a team of specialists – oncologists, surgeons, radiation therapists, and primary care physicians. Coordinating vaccination schedules across these different providers can be a logistical nightmare.
- Access Barriers: Even with a clear plan, physical access to vaccinations can be problematic. This might include issues like limited availability at the oncologist’s office, pharmacy restrictions, or transportation difficulties.
The Role of the Oncologist and Primary Care Physician
Oncologists are at the forefront of cancer care and play a crucial role in advising patients about vaccinations. Primary care physicians also have a responsibility in coordinating care.
- Oncologist’s Responsibilities:
- Patient Education: Providing clear and concise information about the importance of vaccinations and the specific vaccines recommended for their patient’s condition.
- Risk Assessment: Evaluating the patient’s individual risk factors and tailoring vaccine recommendations accordingly.
- Coordination: Communicating with the patient’s primary care physician and other specialists to ensure a unified approach to vaccination.
- Primary Care Physician’s Role:
- Vaccine Administration: Administering vaccines that are not readily available in the oncology clinic.
- Medication Reconciliation: Ensuring that vaccine administration doesn’t conflict with the patient’s current medications or treatments.
- Maintaining Vaccination Records: Keeping up-to-date records of all vaccinations received by the patient.
Navigating Pharmacies and Clinics: Challenges and Solutions
Pharmacies and clinics are vital access points for vaccines, but challenges can arise within these settings.
- Pharmacy Limitations: Some pharmacies may not stock all the necessary vaccines, particularly those tailored for immunocompromised individuals. Communication between the oncologist and the pharmacy is key.
- Clinic Availability: Clinics may have limited hours or appointment availability, making it difficult for patients to schedule vaccinations, especially those undergoing frequent cancer treatments.
- Insurance Coverage: Navigating insurance coverage for vaccinations can be complex, leading to delays or financial burdens for patients.
- Solution: Enhanced Communication and Collaboration:
- Streamlined Referrals: Clear referral pathways between oncology practices, primary care physicians, and pharmacies are essential.
- Centralized Vaccination Records: Using electronic health records (EHRs) to share vaccination information across all providers.
- Patient Advocacy: Healthcare systems can offer patient navigators who can help patients understand the vaccine process and navigate the healthcare system.
The Importance of Nurse Involvement
Nurses play a vital role in patient education and support.
- Patient Education: Nurses are often the first point of contact for patients, providing information about vaccine recommendations, potential side effects, and the vaccination process.
- Vaccine Administration: Nurses administer vaccines and monitor patients for any adverse reactions.
- Advocacy: Nurses advocate for patients to ensure they have access to the vaccinations they need.
Addressing the Systemic Issues
The challenges faced by cancer patients seeking vaccinations are often rooted in systemic issues.
- Lack of Standardization: A lack of standardized protocols and guidelines across healthcare providers can lead to inconsistencies in care.
- Insufficient Training: Healthcare professionals may not always have adequate training on the specific vaccination needs of cancer patients.
- Inefficient Communication Systems: Poor communication between different healthcare providers can result in fragmented care and missed opportunities for vaccination.
Conclusion: Improving Access and Protecting Vulnerable Patients
The experience of one cancer patient seeking vaccination highlights critical areas for improvement within the healthcare system. By addressing the systemic challenges, improving communication, and ensuring better coordination of care, we can significantly enhance access to life-saving vaccinations for vulnerable individuals. This requires a concerted effort from all healthcare providers – doctors, nurses, pharmacists, and clinics – to prioritize patient well-being and create a more seamless and supportive vaccination experience. Ultimately, the goal is to protect cancer patients from preventable diseases and improve their chances of survival and quality of life.
Frequently Asked Questions (FAQs)
Why are vaccinations so important for cancer patients? Cancer patients often have weakened immune systems due to the disease itself or treatments like chemotherapy and radiation. Vaccinations help protect them from potentially serious infections that could lead to hospitalization or even death.
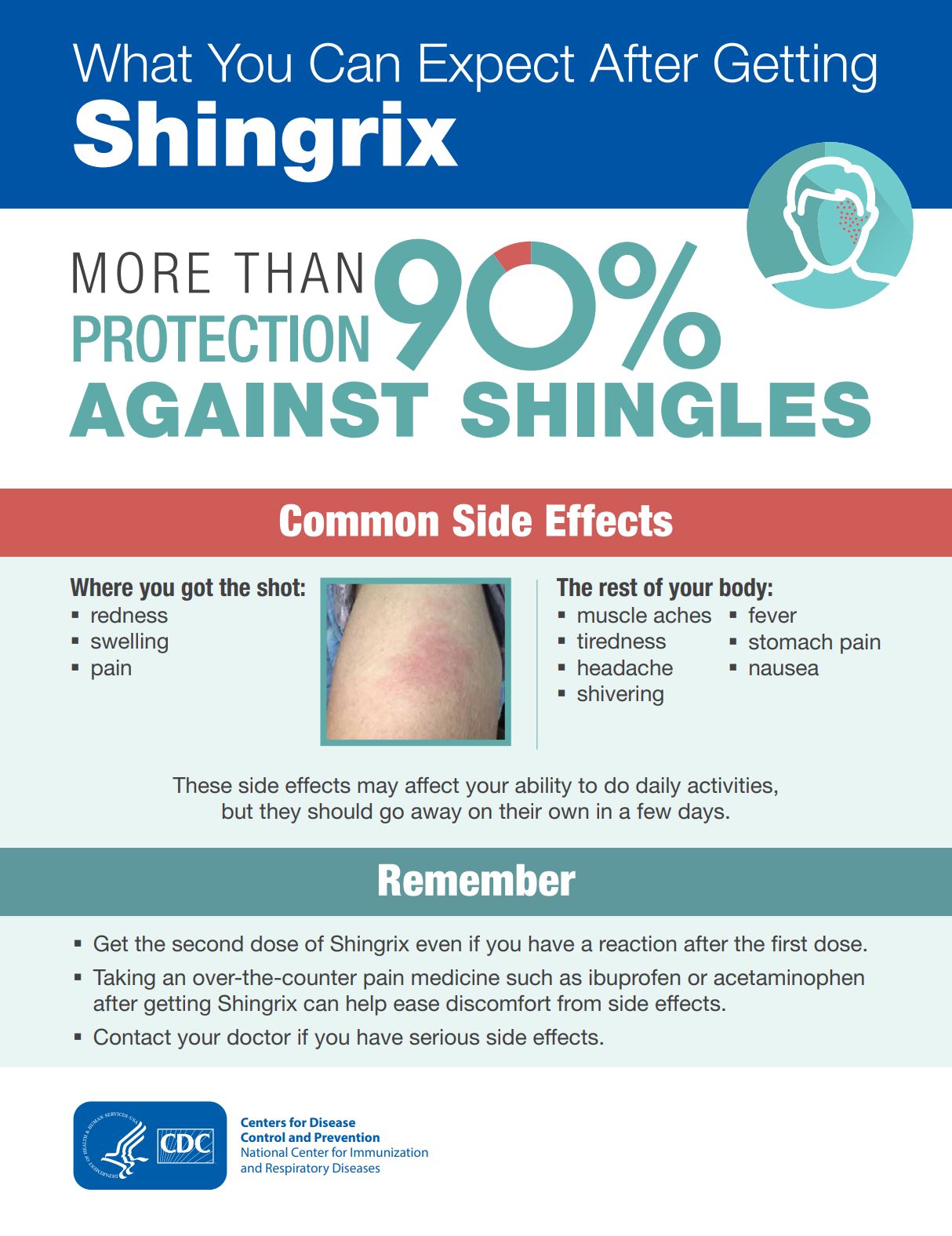
What vaccines are typically recommended for cancer patients? Recommendations vary depending on the type of cancer, treatment plan, and individual patient factors. Common vaccines include the influenza (flu) vaccine, the pneumococcal vaccine (to protect against pneumonia), and potentially vaccines against shingles and other diseases. Your oncologist will provide the best advice.
Where can cancer patients get vaccinated? Vaccinations may be available at your oncologist’s office, your primary care physician’s office, pharmacies, or local health clinics. It’s best to discuss the options with your healthcare team to find the most convenient and appropriate location for you.
What should I do if I’m a cancer patient and I’m unsure about which vaccines I need? The best course of action is to consult with your oncologist or primary care physician. They can assess your individual needs and provide personalized recommendations. Don’t hesitate to ask questions about the risks and benefits of each vaccine.
Are there any vaccines that cancer patients should not receive? Yes, some vaccines containing live attenuated viruses (weakened but live viruses) may not be safe for cancer patients, especially those undergoing chemotherapy or with weakened immune systems. Your doctor will advise you on which vaccines are suitable for you.