Perimenopause and Cancer Risk: Why This Transition Matters More Than Expected
Perimenopause, the transitional phase leading up to menopause, is often characterized by irregular periods, hot flashes, and mood swings. While these symptoms dominate the conversation, a less discussed but equally crucial aspect is the potential impact on cancer risk. This transitional period is more than just hormonal fluctuations; it represents a significant shift in the body’s physiology that can influence susceptibility to several types of cancer. Understanding this connection is crucial for proactive health management.
Hormonal Shifts and Cancer Risk: A Complex Relationship
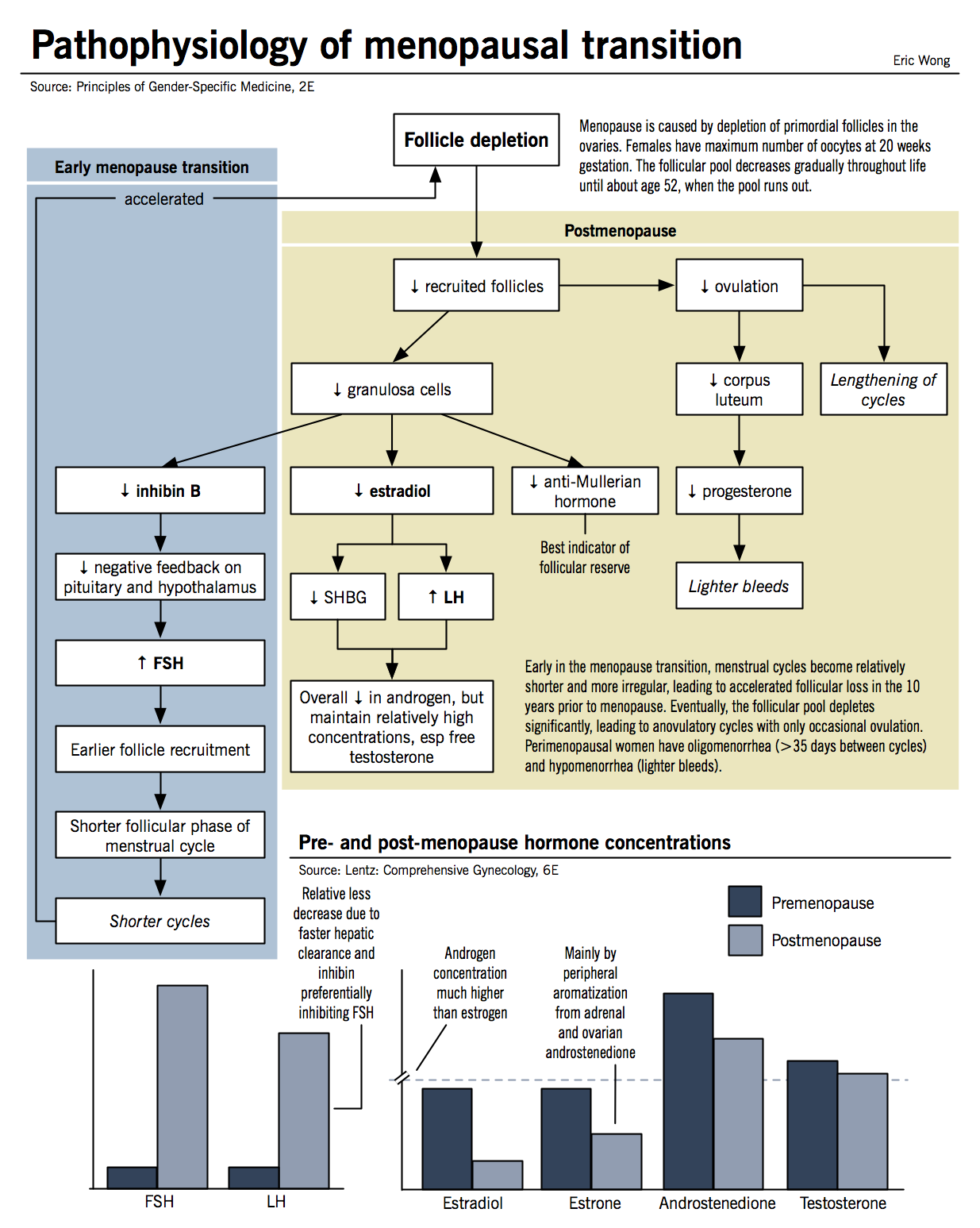
The hormonal rollercoaster of perimenopause significantly alters the body’s internal environment. Fluctuating estrogen and progesterone levels, alongside changes in other hormones, can influence cellular growth and development, impacting the risk of certain cancers. This isn’t a simple cause-and-effect relationship; the influence is complex and varies depending on several factors, including:
- Type of Cancer: The relationship between perimenopause and cancer risk differs across various cancer types. Some cancers, like breast cancer, may see a slightly increased risk during this transition, while others may show a decrease or no significant change.
- Genetic Predisposition: Family history of cancer significantly influences individual risk, regardless of perimenopause.
- Lifestyle Factors: Smoking, diet, exercise, and alcohol consumption all play a critical role in modulating cancer risk throughout a woman’s life, including during perimenopause.
- Ethnicity and Race: Variations in genetic makeup and environmental exposures can influence cancer risk across different ethnic and racial groups.
Breast Cancer and Perimenopause: A Closer Look
Breast cancer is a primary concern during perimenopause. While estrogen is often implicated in breast cancer development, the fluctuating levels during this transition can create a complex scenario. The exact impact remains a subject of ongoing research, but maintaining regular breast self-exams and mammograms is crucial.
Other Cancers and Perimenopause
While breast cancer receives the most attention, perimenopause can also subtly influence the risk of other cancers, including:
- Endometrial Cancer: Changes in estrogen and progesterone levels can impact the uterine lining, potentially increasing the risk of endometrial cancer.
- Ovarian Cancer: The relationship between perimenopause and ovarian cancer is less clear-cut, but the cessation of ovulation may play a role.
Proactive Steps for Cancer Prevention During Perimenopause
Given the complex interplay between perimenopause and cancer risk, proactive health management is essential. This includes:
- Regular Check-ups: Schedule routine visits with your gynecologist for monitoring and discussions about cancer screening.
- Healthy Lifestyle Choices: Maintaining a balanced diet, engaging in regular physical activity, limiting alcohol consumption, and avoiding smoking are crucial for overall health and cancer prevention.
- Early Detection: Familiarize yourself with the signs and symptoms of various cancers and seek medical attention promptly if any concerns arise.
- Genetic Counseling: If you have a family history of cancer, genetic counseling can help assess your individual risk and guide preventative strategies.
Conclusion
Perimenopause is a significant life transition impacting more than just menstrual cycles and hot flashes. Understanding its potential influence on cancer risk empowers women to make informed decisions about their health. By prioritizing regular check-ups, adopting a healthy lifestyle, and being aware of potential risks, women can navigate this phase with greater confidence and proactively protect their long-term well-being. Open communication with healthcare providers is vital for personalized guidance and tailored cancer prevention strategies.
FAQs
Q1: Does perimenopause definitively cause cancer?
A1: No, perimenopause doesn’t directly cause cancer. However, the hormonal shifts during this transition can modify the risk of developing certain cancers, making it a crucial period for proactive health management.
Q2: When should I start getting screened for cancer during perimenopause?
A2: Screening recommendations vary based on individual risk factors, family history, and age. Discuss appropriate screening schedules with your healthcare provider.
Q3: Can hormone replacement therapy (HRT) influence cancer risk during perimenopause?
A3: HRT can influence cancer risk, with some studies suggesting potential increased risks for certain cancers. The decision to use HRT should be made in consultation with a healthcare professional, carefully weighing the benefits and risks based on individual circumstances.
Q4: Is there a specific diet to reduce cancer risk during perimenopause?
A4: A diet rich in fruits, vegetables, whole grains, and lean protein, while limiting processed foods, red meat, and sugary drinks, is generally recommended for overall health and cancer prevention.
Q5: What are the early warning signs of cancer I should be aware of?
A5: Early warning signs vary depending on the type of cancer. Common signs can include unexplained weight loss or gain, persistent fatigue, unusual bleeding or discharge, lumps or bumps, and persistent changes in bowel or bladder habits. Consult your doctor if you experience any concerning symptoms.