Parkinson’s Disease: Could the Gut Be the Culprit? Scientists Explore Extra-Brain Origins
Parkinson’s disease, a debilitating neurodegenerative disorder, is traditionally understood as a brain-based illness. However, groundbreaking research is challenging this long-held belief, suggesting that the disease’s origins might lie outside the central nervous system, potentially in the gut. This article delves into the emerging evidence supporting the extra-brain origins hypothesis and its implications for diagnosis and treatment.
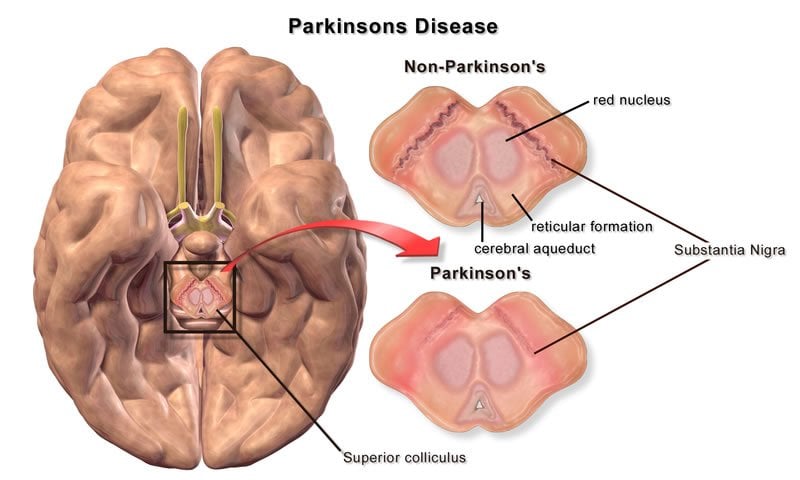
The Traditional View: Parkinson’s in the Brain
For decades, the hallmark of Parkinson’s has been the degeneration of dopamine-producing neurons in the substantia nigra, a region deep within the brain. This neuronal loss leads to the characteristic motor symptoms, including tremors, rigidity, slow movement (bradykinesia), and postural instability. Treatment has primarily focused on managing these symptoms within the brain, often through dopamine replacement therapy.
The Emerging Evidence: A Gut-Brain Connection
Recent studies have revealed a compelling connection between the gut and Parkinson’s disease. This “gut-brain axis” is a complex bidirectional communication network linking the gastrointestinal system and the brain via the vagus nerve and other pathways. Evidence supporting an extra-brain origin includes:
- Alpha-synuclein aggregation: Alpha-synuclein is a protein implicated in Parkinson’s. Studies have shown that abnormal clumps of alpha-synuclein can accumulate in the gut before appearing in the brain. This suggests a potential “prion-like” spread from the gut to the brain.
- Gut microbiome dysbiosis: Changes in the composition and function of the gut microbiome (the community of microorganisms living in the gut) have been observed in individuals with Parkinson’s. These imbalances may contribute to inflammation and neuroinflammation, ultimately impacting brain health.
- Vagus nerve involvement: The vagus nerve, a major communication pathway between the gut and the brain, may play a crucial role in the spread of alpha-synuclein and the development of Parkinson’s. Vagotomy (surgical removal of part of the vagus nerve) has been associated with a reduced risk of Parkinson’s in some studies.
- Gastrointestinal symptoms: Many individuals with Parkinson’s experience gastrointestinal issues such as constipation, nausea, and loss of appetite years before the onset of motor symptoms. This suggests that gut dysfunction may be an early indicator of the disease.
Implications for Diagnosis and Treatment
The growing evidence for an extra-brain origin of Parkinson’s has significant implications for both diagnosis and treatment. Early detection of gut-related issues might allow for earlier intervention and potentially delay or even prevent the onset of motor symptoms. Future research may focus on:
- Developing gut-targeted therapies: These could aim to modulate the gut microbiome, reduce alpha-synuclein aggregation, or protect the gut-brain axis.
- Improving diagnostic tools: Identifying gut-related biomarkers could provide earlier and more accurate diagnosis of Parkinson’s.
- Exploring preventative strategies: Modifying diet, lifestyle, and gut health might help reduce the risk of developing Parkinson’s.
Conclusion
While the exact origins of Parkinson’s disease remain a subject of ongoing research, the evidence increasingly points towards a significant role for the gut. This paradigm shift necessitates a broader perspective on the disease, encompassing the gut-brain axis and exploring new avenues for diagnosis, prevention, and treatment. Further research is crucial to unravel the intricate mechanisms involved and translate these findings into effective clinical strategies.
Frequently Asked Questions (FAQs)
Q: Does this mean Parkinson’s is caused by gut problems? A: The research suggests a strong association between gut health and Parkinson’s, but it doesn’t necessarily mean gut problems directly cause the disease. More research is needed to understand the causal relationship.
Q: Can I prevent Parkinson’s by improving my gut health? A: Maintaining a healthy gut microbiome through a balanced diet, regular exercise, and stress management may reduce your risk of developing Parkinson’s, but it’s not a guaranteed preventative measure.
Q: What kind of gut-related symptoms should I watch out for? A: Persistent constipation, changes in bowel habits, nausea, and loss of appetite, especially if occurring years before the onset of motor symptoms, warrant medical attention.
Q: Are there any current treatments targeting the gut for Parkinson’s? A: Currently, no treatments specifically target the gut for Parkinson’s. However, research is actively exploring this area, with promising avenues being investigated.
Q: Should I get my gut microbiome tested if I’m worried about Parkinson’s? A: While testing the gut microbiome may become a standard diagnostic tool in the future, it’s currently not a routine test for Parkinson’s. Consult your doctor to discuss your concerns and potential testing options.